
At the NourishED Summit, I had the opportunity to share our perspective on the evolving landscape of regulated psychedelic therapy in the United States. While much of the public conversation is about clinical trials and pharmaceutical pipelines, state-regulated programs are already shaping how people access these therapies. They are new and imperfect, but they are also real, and they offer lessons about where the field is headed.
We are living through a unique moment. On one track, pharmaceutical companies are racing through the FDA approval process. More than sixty trials are underway, half of them in Phase 3 or beyond. Compass Pathways has psilocybin in late-stage trials, MAPS has brought MDMA to the edge of approval, and ketamine has already established itself as one of Janssen’s fastest growing drugs. Psychiatry has not seen many new tools in decades, and the promise of psychedelic-inspired medicines has created significant momentum.
On another track, states are building their own frameworks. Oregon became the first state to launch a legal psilocybin program in 2023. Colorado followed in 2025 with a model that allowed clinicians such as social workers and psychiatrists to integrate psilocybin therapy into their licenses, creating a closer bridge to mainstream behavioral health. New Mexico is preparing to launch its program in 2027. These are not medical marijuana programs and they are not pharmaceutical pathways. They are something new: state-level experiments in supervised adult use with therapeutic intent.
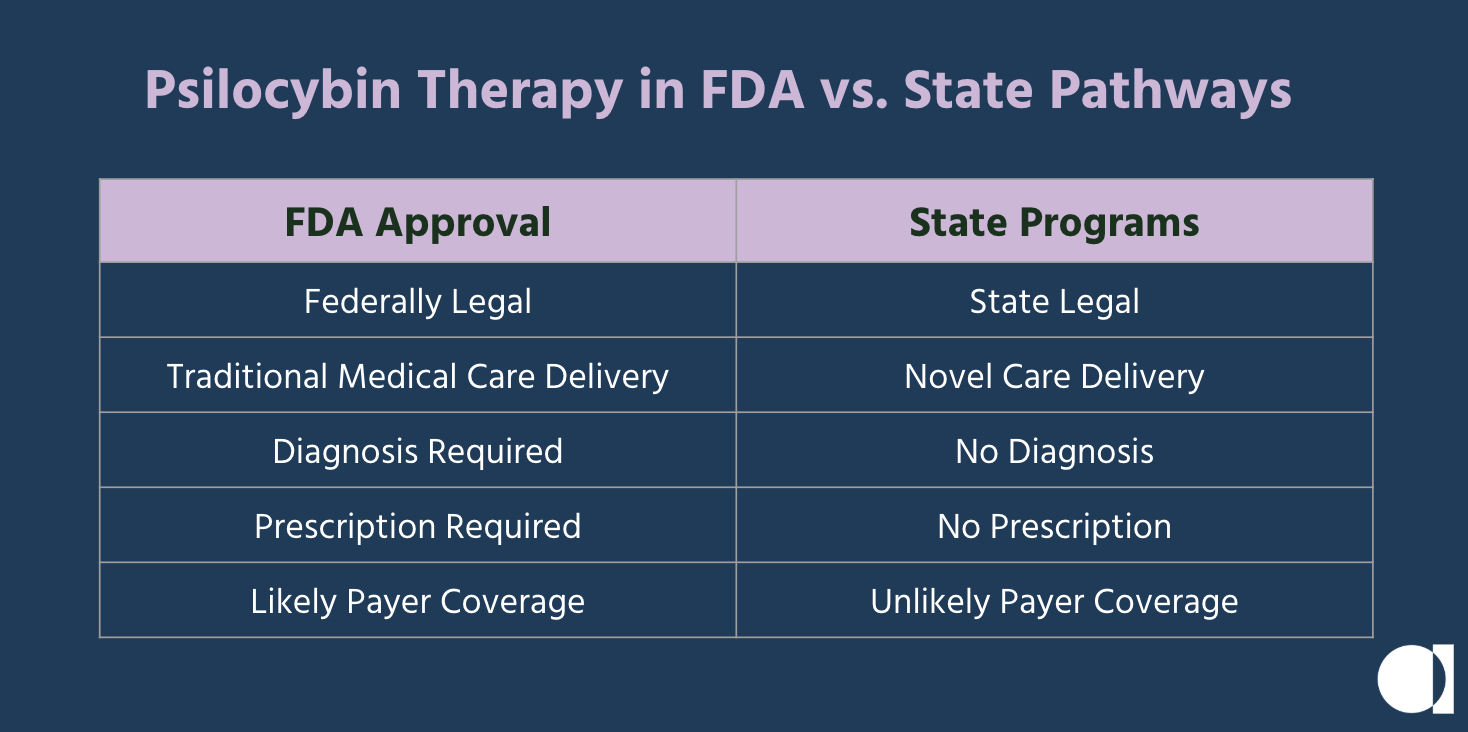
The urgency behind these programs comes from people who could not wait a decade for FDA approval. Tens of millions of Americans live with depression, anxiety, PTSD, and addiction. Research from leading universities has shown psilocybin’s safety and potential, and grassroots coalitions of patients, families, therapists, and veterans pushed ballot measures forward. Cannabis offered a precedent, showing that state-level change could pave the way for broader reform. And unlike the FDA model, which will be tied to narrow diagnoses and prescriptions, state programs allow access for a broader range of intentions including mental health, spiritual growth, and personal development.
To understand how these programs work, it helps to follow the client journey.
- It begins with discovery, where education and trust-building play a role in moving someone from curiosity to readiness.
- Preparation involves medical and psychological screenings, informed consent, and support systems.
- The psilocybin therapy administration session itself often takes place in a licensed center, with 4-6 hours of guidance from trained facilitators using lab-tested medicine.
- Finally, integration helps the insights take root through therapy, community, and ongoing practice.
Along this journey, facilitators, centers, cultivators, labs, and product makers form a new kind of locally-regulated health ecosystem.
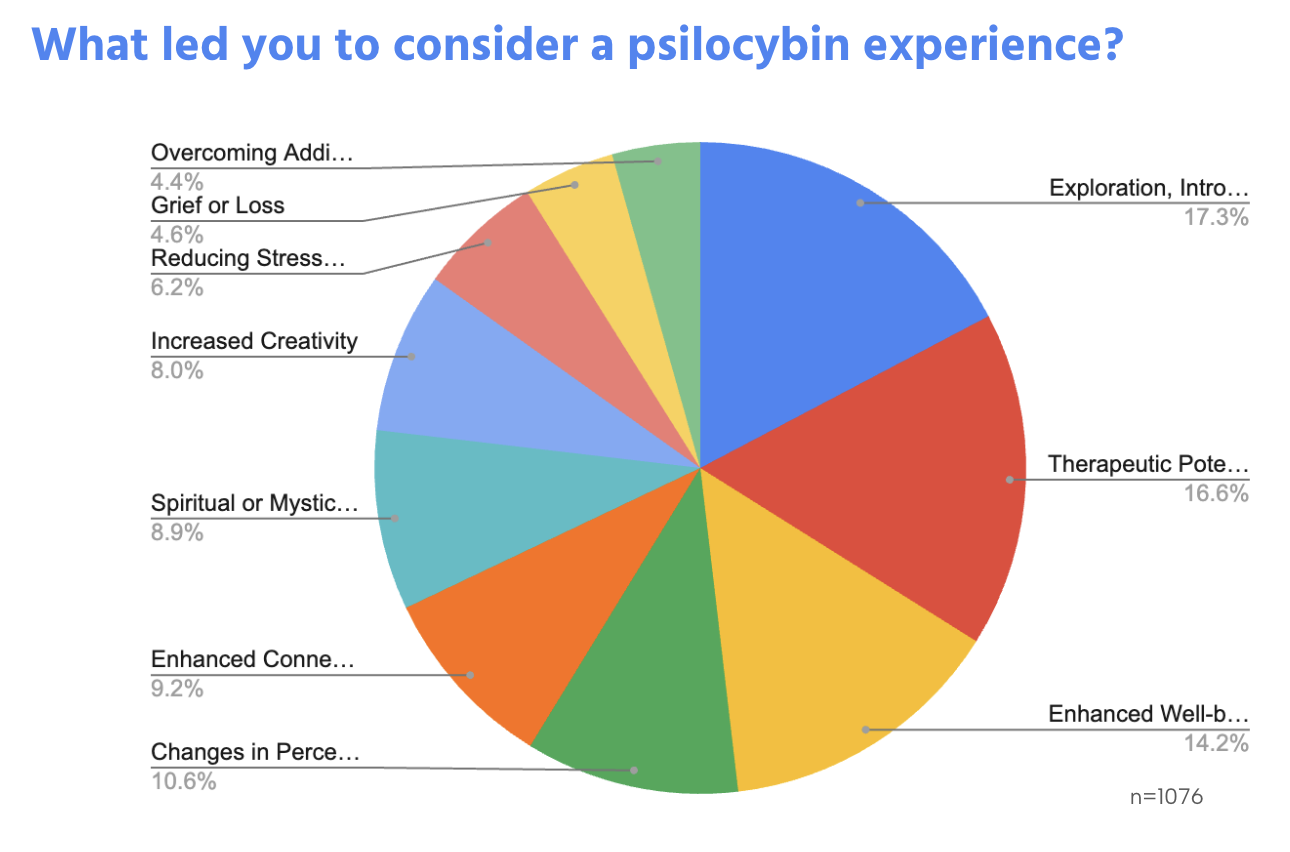
Why do people seek out psilocybin therapy? Our data from more than a thousand journeys shows that exploration, introspection, and personal growth are cited just as often as clinical motivations. Many people travel to Oregon and Colorado from out of state to participate, and the outcomes they report are consistently strong. Safety scores are high, facilitators receive near-unprecedented net promoter ratings, and the benefits are widely endorsed by participants.
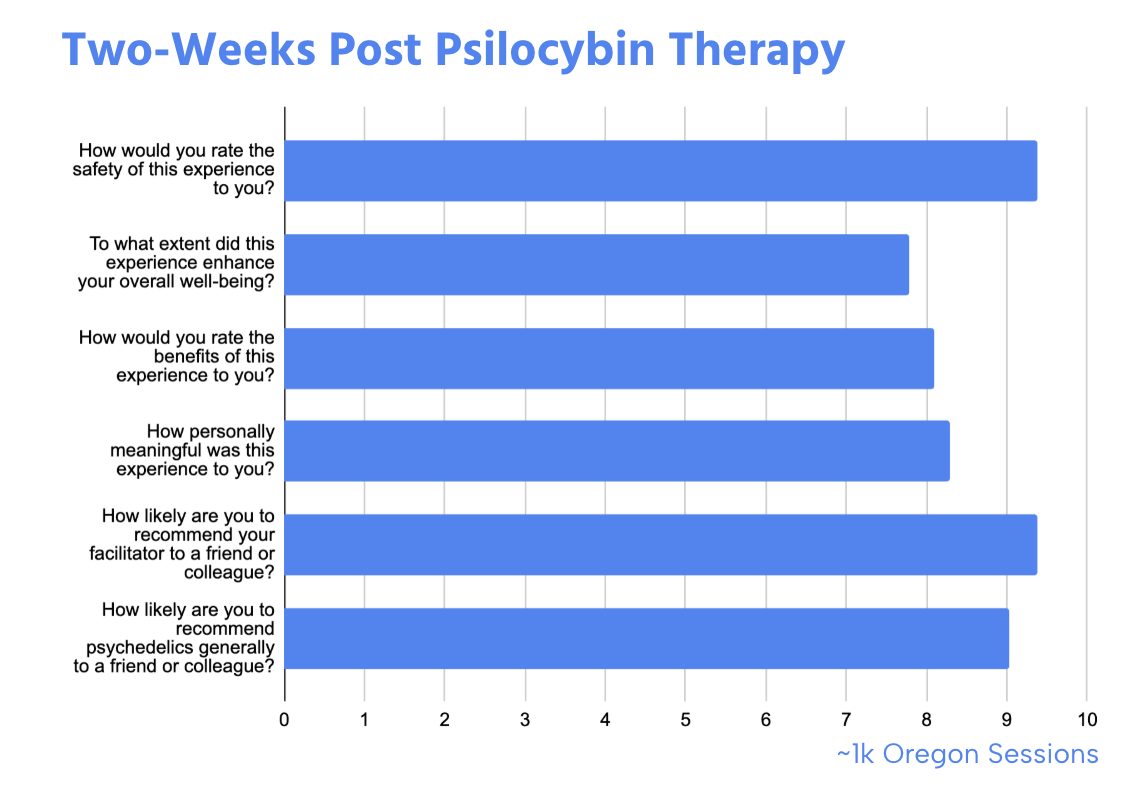
Yet the programs are struggling. Oregon, for example, has already seen more than a third of its service centers close. The barriers are clear. Sessions are expensive, averaging $2,500, which limits access to those with means. Awareness is low, with fewer than one in five Oregonians with a relevant diagnosis even knowing the program exists. Compliance adds layers of cost and paperwork, while market fragmentation means that seekers often cannot find providers, and providers cannot find clients. A Google search for “psilocybin therapy depression” will not produce a single regulated provider within the first nineteen pages of results.
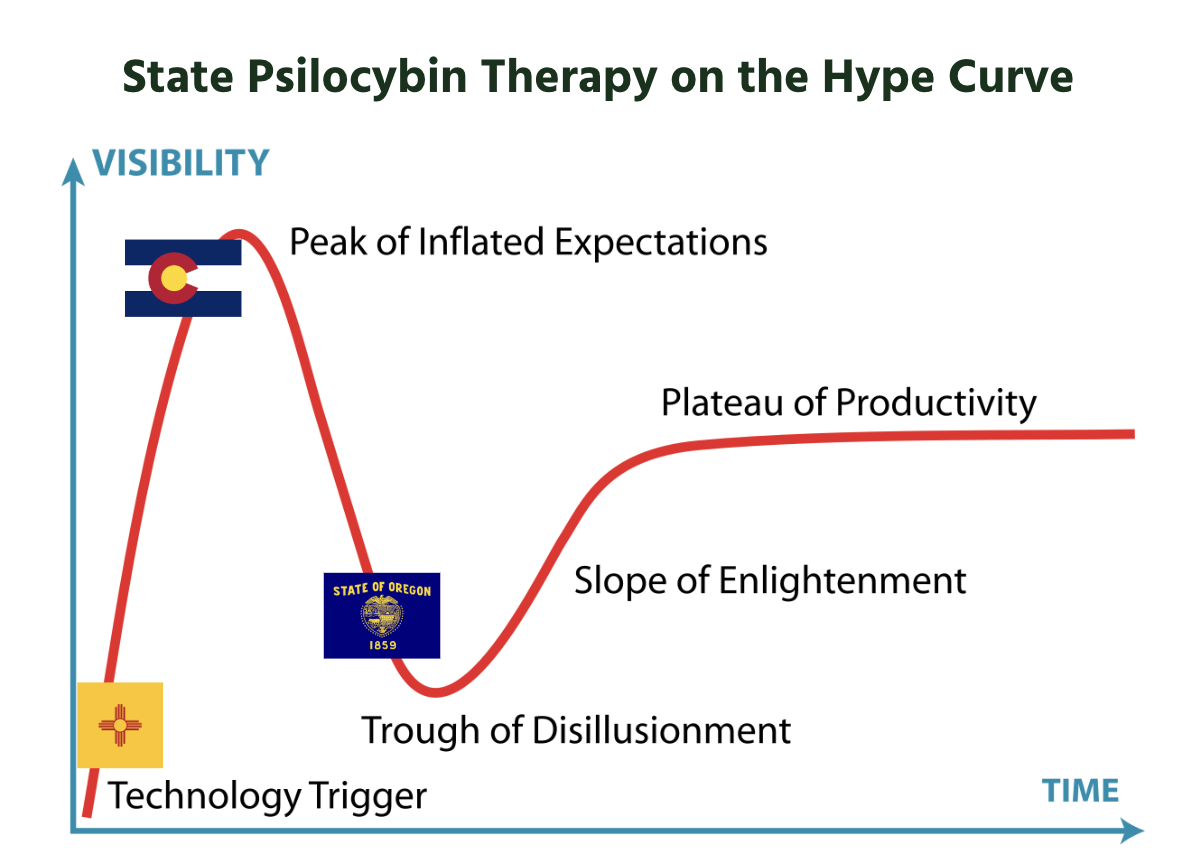
These challenges are not reasons to dismiss the programs. They are signs of a market still finding its footing. If Oregon is in the trough of disillusionment, the path forward is to climb the slope of enlightenment. That means building referral pathways from existing care providers so psychedelics can be integrated rather than siloed. It means normalizing access so that curiosity can lead to care without getting lost in confusion. It means driving down costs, exploring group models, and eventually unlocking insurance coverage. Most of all, it means generating real-world evidence to inform regulators, insurers, and policymakers.
My vision for 2028 is that psychedelic therapy becomes a federally recognized standard of care for both mental health and personal growth. It will be delivered in coordinated systems where clinicians, facilitators, and clients work together in trust and safety. Infrastructure companies like Althea will play a quiet but essential role, ensuring that compliance, payments, and data systems are in place to support this transition.
The call to action is simple. Share stories to reduce stigma. Clinicians should build referral pathways and learn the protocols. Policymakers should support frameworks that prioritize safety and access. With the right coordination, psychedelic therapy can move from being profoundly personal to being profoundly available.


